What to Do if You're Still Depressed After 30 Years
Depression is a serious condition that can become chronic and disabling. It can turn your life upside down in a matter of weeks. While many people with depression live happy, healthy lives, certain forms of depression may last for decades.
If your depression has lasted for 30 years or more, you may be frustrated, hopeless, or overcome by symptoms. You may have tried several medications or exhausted multiple coping skills. If that’s you, it’s important to know what treatment options will work.
Every year, more people are learning to manage chronic depression by learning about the abundance of treatment approaches available. Identifying the best approaches will help you avoid hospitalizations and put you on the path to stability and remission.
An overview of chronic depression
The definition of chronic depression has evolved since the introduction of the DSM-5-TR. The manual includes persistent depressive disorder (PDD), which describes an ongoing form of depression that never disappears. Another form of depression isn’t referenced in the manual. It’s called treatment-resistant depression (TRD), which refers to depression that doesn’t respond to medications. Both disorders involve chronic depressive symptoms, and both are known to impair normal functioning.
What is persistent depressive disorder (PDD)
Persistent depressive disorder, also known as dysthymia, is a chronic mental illness that includes depressive symptoms that last for at least two years (or one with children and adolescents). With PDD, you may be suicidal more frequently. You’ll also be depressed most of the time and experience at least two of the following symptoms:
- You feel hopeless
- You have low self-esteem
- You have trouble concentrating or making decisions
- You have low energy or feel fatigued
- Your appetite is poor or you’re overeating
- You have trouble sleeping or you’re sleeping too much
To meet PDD’s diagnostic criteria, your symptoms must impair your ability to work or function socially. Your depression will have been caused by one of many factors, including relationship problems, abuse, or childhood neglect. Your symptoms will be milder than with Major Depressive Disorder (MDD), and both psychotherapy and medication will have proven ineffective.
What is treatment-resistant depression (TRD)?
A chronic form of depression called treatment-resistant depression, or TRD, is another form of depression that doesn’t disappear. It’s characterized by an inadequate response to two or more antidepressants. With TRD, the lack of responsiveness to medication occurs even with therapy. The symptoms are like MDD. However, they’re unique because they’re chronic and don’t respond to common treatments.

With TRD, you’ll feel sadness and low energy. You’ll likely have low self-esteem and hopelessness, and will have lost interest in activities you once enjoyed. Not only will your symptoms have impaired normal functioning, you may also be among the diagnosed that experiences a greater economic burden given the frequency of psychiatric admissions and emergency room visits.
What if depression doesn’t go away for decades?
Depression that won’t go away will have a major impact on your life. It may leave you socially isolated or seeing strain in your relationships. You’ll likely struggle at work or school, and have intense suicidal thoughts. These issues make life unbearable even with treatment. Only through the pursuit of less-common treatments will you have a better chance of overcoming chronic depression.
Less common treatments may help you in ways that common treatments won’t:
- They may offer rapid, temporary relief
- You might see stability restored faster
- They may alter consciousness to reduce symptoms
- They may target neurotransmitters that antidepressants don’t
With communication, less common approaches may increase your chances of success in your recovery. These options require patience, but remission is possible. You may find it helpful to browse literature featuring success stories. You may also benefit from talking to your psychiatrist about your prognosis.
To improve your prognosis, it’s important to understand how your coping mechanisms must change. Chronic depression requires a more committed, active approach, which involves the application of self-management techniques known to help you achieve remission.
Practice self-management
Treating chronic depression requires a higher tier of treatment than with MDD. To achieve remission, you’ll need a proactive, focused effort that involves routine communication, as well as active support from supporters outside of the system. You’ll need to utilize a self-management approach, which refers to the regulation, monitoring, and assessment of thoughts, behaviors, and symptoms. The purpose of self-management is to help you achieve full remission, as well as obtain long-term stability and healthy life functioning.
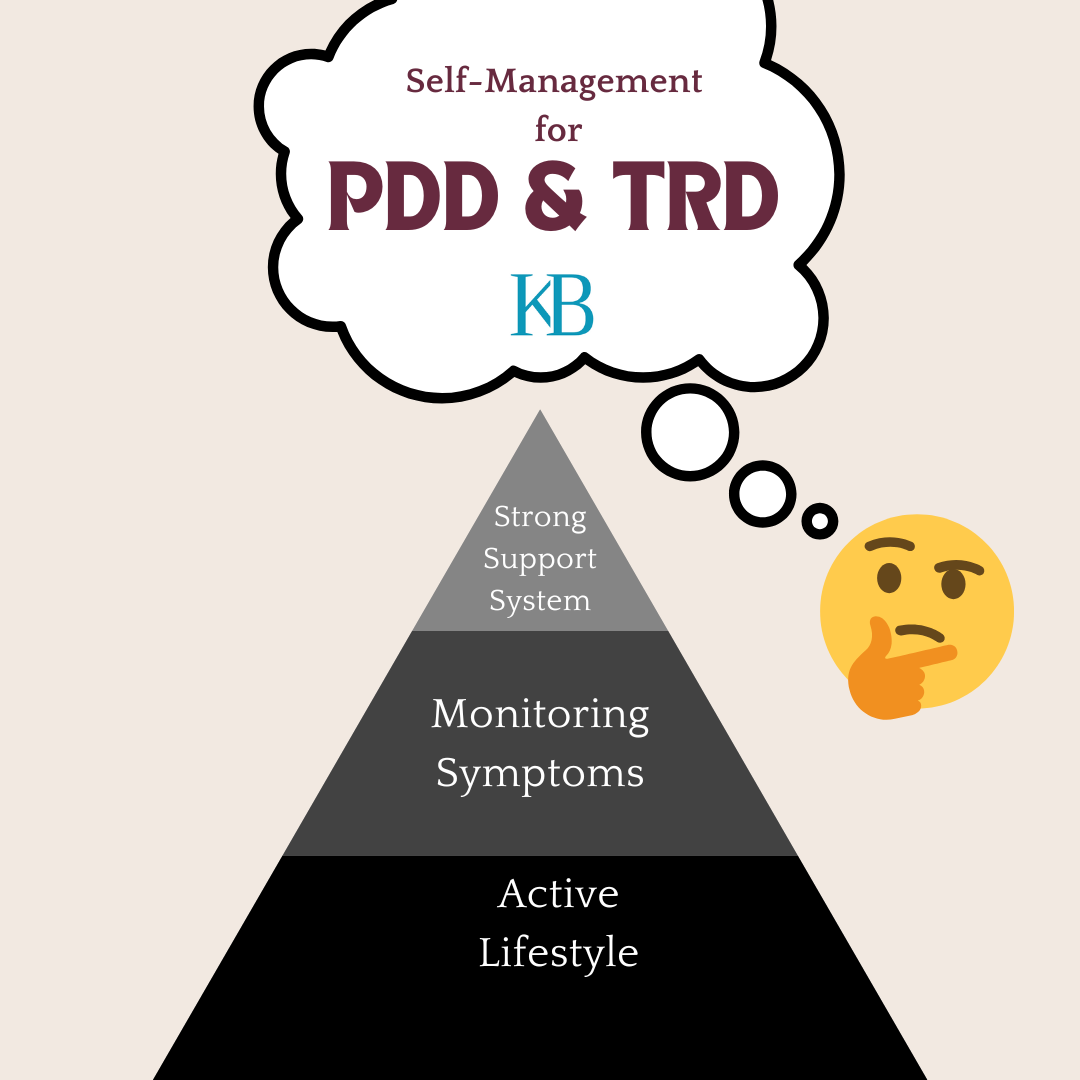
Monitor symptoms proactively
With chronic depression, you’ll use an active approach to monitoring and coping with symptoms. You’ll achieve this by recording your thoughts, feelings, symptoms, and changes in behavior in a recovery journal. A journal lets you stay attentive to patterns, while also improving your chances of improving your thoughts and emotions.
You might try:
- Recording dates and times when you experience symptoms
- Noting patterns while recording your emotions and thoughts
- Using diagrams, charts, or pictures to go into depth
- Identifying triggers or stressors and describing them in detail
- Identifying what you’ve learned about your symptoms over time
- Recording details on how your symptoms affect your life
Journaling about symptoms has proven benefits. However, the actual effectiveness of journaling for depression is unclear. Studies show journaling efficacy is measured by its supplementary benefits, meaning it’s most helpful when used along with other evidence-based treatments.
Believe in your ability to live well
Managing chronic depression involves acknowledging your unique strengths and gifts, ideally, for the purpose of self-empowerment. Believing you can change, adapt, thrive, and bounce back is key to restoring functioning in all areas of your life.
Embracing an optimistic belief mindset means you identify times where you were in crisis, but overcame your symptoms. You’ll recall times where your depression was at its worst, yet you found a way to manage. You’ll reflect on various treatments that you can pursue and the support you have available. You’ll consider the effort required, and the resources and strengths you’ll draw on to for stability. The point of this process is to change your thoughts from negative to hopeful, and to bring balance to your life through the acknowledgment of success stories in your community.
Through your commitment to your treatment plan and the recognition of resilience you’ve acquired, you’ll learn living well is possible if you focus on hope and opportunity.
Form a strong bond with your support system
Mental health professionals refer to your support system as informal caretakers. They serve as the foundation for remission because they provide basic forms of support, whether tangible, emotional, or financial. Your support system will also be present when your therapist or counselor is not. They may be in more frequent contact with you and likely know your personality and illness better.
This isn’t always the case, however. Contrarily, a closer, more meaningful relationship with your support system is a must. Research shows that a close support network is essential in preventing mental health problems. The closer you are to your support network, the more likely you are to maintain good health. A strong bond with your support network also facilitates recovery, either directly through recovery-related communities, or indirectly through peer-support groups or digital support platforms.
Maintain an active lifestyle
To improve with chronic depression, you’ll need to engage in an active lifestyle. Action, however challenging, is a key component of enjoying life to the fullest, reducing the severity of symptoms, and bringing balance to your life through the application of regular, consistent participation in activities.
Research shows that action-oriented coping skills are among the most dependable coping strategies. These coping skills include meaningful activities that instill purpose in your behaviors, as well as routine exercise and deep, reflective social engagement.
Recreation, exercise, and social engagement
Recreation involves fun, enjoyment, hobbies, and excitement. But with chronic depression, finding the drive to participate may be overly demanding. Filling these pastimes with purpose is the best approach for finding motivation. Doing so will help you sustain the length of application.
Creating purpose in recreation requires any of the following actions:
- Getting involved in activities that inspire creativity
- Choose activities where you can identify specific gains
- Participate at times when symptoms are more or less severe
- Pursue activities that involve physical stimulation or adventure
- Engage in activities that involve groups or crowds
Activities must require imagination or exertion, while creativity opens up the mind and reduces symptoms through expression. Creativity also allows for improved social functioning in group settings. In addition, the pursuit of activities at times when symptoms are less severe will extend the times you’re finally symptom free, or alleviate those symptoms when they become too severe. Finally, engagement in recreation with groups will bring added relief. Plus, you’ll enjoy companionship, and support, when you’re having fun around people.
Choose less common treatments
Less common treatments represent hope for people living with chronic forms of depression. These treatments include rapid-acting psychedelics, long-lasting brain stimulation therapies, and integrative care therapies that respond when medication and treatment won’t.
Researchers have investigated these treatments and discovered that they’re helpful. You’ll benefit from discussing these treatments in session with your therapist or psychiatrist.
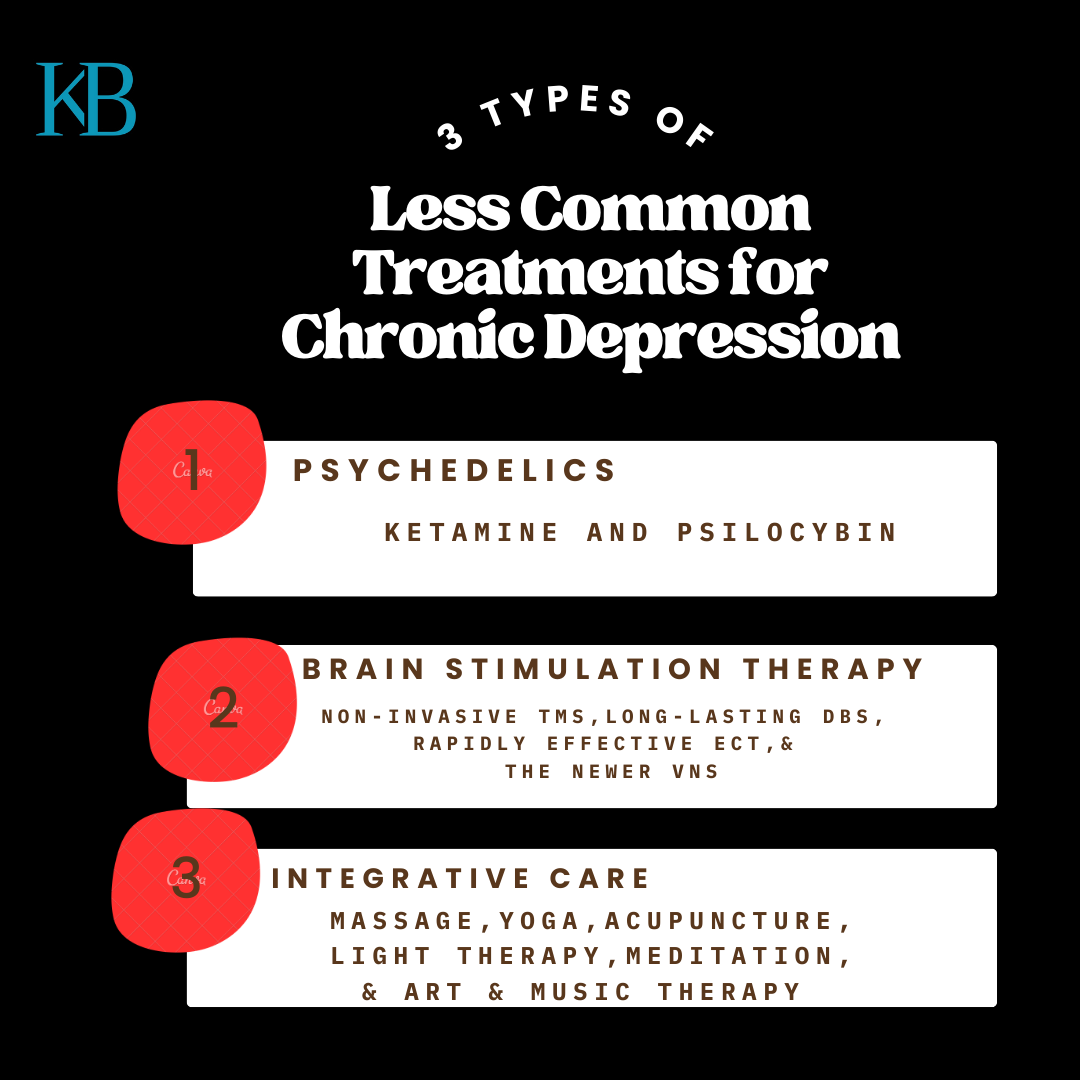
Psychedelics for immediate relief
Researchers have discovered that certain recreational drugs show promising effects for treating chronic depression. One of those drugs is ketamine, an anesthetic that doctors use in emergency settings to maintain patients’ stability. While ketamine can be abused and isn’t recommended for long-term use, the form known as esketamine is approved to help with TRD.
Studies show a single dose of ketamine treatment can provide immediate, temporary relief from depression, proving effective for up to 3–7 days. Ketamine is available in clinical settings. It’s also available as a nasal spray. when prescribed by a licensed healthcare provider.
Another type of psychedelic, psilocybin, is responsible for increasing global integration, meaning the drug targets neurotransmitters in the brain to create flexibility in thinking patterns. If you have chronic depression, psilocybin is known to open your mind, which cuts down on long periods of dark, negative thinking.
After taking psilocybin, you may notice a positive shift in thinking right away. You may also see a sustained improvement in symptoms after six weeks. Going forward, you should monitor changes in your symptoms and behavior and avoid taking psychedelics without the support of a psychiatrist.
Brain stimulation therapies for long-lasting success
Using electrodes implanted in various parts of the brain, this form of therapy uses surgically implanted electrodes that send electrical impulses to the brain. Brain stimulation therapy disrupts abnormal activity in the brain, and when combined with therapy, is proven to be effective.
Recent studies show a response rate of 60% for people with treatment-resistant or persistent forms of depression. A response rate refers to the percentage of people that benefit from a form of treatment. The research indicates that while brain stimulation therapy is effective, it’s recommended as an option only for people who don’t respond to more common treatments.
Specific types of brain stimulation therapies include:
- The non-invasive Transcranial Magnetic Stimulation therapy (TMS)
- The newer Vagus Nerve Stimulation therapy (VNS)
- The long-lasting Deep Brain Stimulation therapy (DBS)
- The rapidly effective Electroconvulsive therapy (ECT)
To receive treatment, talk to your psychiatrist. They’ll want to check and see if your insurance provides coverage. Specialists will render the treatment at a special brain stimulation center. The good news is that you can expect results in between 2–4 weeks.
Recent studies show that among five patients who completed a five-year follow-up, four saw long-term success–a noticeably high reduction in symptoms (81%). The long-term efficacy indicates a significant advantage for you if you have chronic depression. You’ll have a better chance of returning to normal functioning, and for a longer period of time.
Integrative care for no side effects
These therapies involve a more natural approach to treatment that doesn’t involve medication. With integrative therapies, the goal is to improve the mind-body connection through gentle, guided exercises. Treatment options include mindfulness-meditation, yoga, art and music therapy, acupuncture, and massage. Also, exposure to light therapy is proven to help.
These options are less expensive and easier to access. Plus, they don’t include side effects you may notice with medication. You can try integrative therapies at your own convenience, which gives you added flexibility and control over your treatment.
Live well with chronic depression
Chronic depression causes depressive symptoms to last for years, and in some cases, for 30 years or longer. The frustration it causes may leave you feeling like no treatment option will work, but communicating with your psychiatrist is a crucial part of finding stability.
Researchers continue to find new treatments and to affirm the benefits of existing options. The goal is to help people like yourself find relief when no other option helps.
Still, living well with chronic depression requires a multi-faceted approach that involves proactive self-management, persistence and patience. With a well-established commitment, extended remission is possible. Every day, people recover successfully. The more society continues to learn, the more opportunities you’ll have to be free from chronic depression.
Kevin Brown is a freelance mental health writer. He lives and writes from Maryland. For more great stories and information about mental health, visit Kevin’s website at www.kevinbwriting.com.

0 Comments Add a Comment?